 Search
Search



Since March 2020, hospitals and health systems nationwide have faced unprecedented financial challenges amid lost revenue and new expenses as they care for their communities in response to COVID-19. The American Hospital Association estimates the total COVID-19 financial impact on providers through June will exceed $200 billion — an average of more than $50 billion a month — with the bulk of losses stemming from canceled elective and nonelective surgeries.1
To help mitigate these financial headwinds, the federal government has thus far created several funding mechanisms through four pieces of legislation to support and reimburse providers for increased costs and lost revenues linked to COVID-19. The most significant sources of health system funding include:
But applying for relief funds is an extremely complex process, exacerbated by overlapping eligibility activities and varying degrees of rigor and documentation. Such is the case for both new efforts like HHS’ Provider Relief Fund and the FCC’s telehealth program, as well as for more established FEMA processes.
For example, FEMA public assistance is designed as a recovery program to help communities to rebuild post-disaster, but COVID-19 is an ongoing crisis with vastly different complexities. While FEMA has strived to establish COVID-specific policies and guidance, there remain nuances particular to how health systems procure supplies, structure labor, account for medical insurance, and more.
These differences require expertise in interpreting guidelines and developing applications that align with FEMA’s current framework, all of which must be properly structured and presented to providers’ state emergency management agencies at a time of unprecedented uncertainty. Reimbursement delays can be expected for providers unable to present their claims in the FEMA-prescribed manner.
Moreover, coordination of benefits across all available grants is critical to identify applicable funding sources based on eligibility criteria; flag potential duplication of benefits; and track application status, receipt of funds, and days to repayment (if applicable). HHS has clearly stated that relief funds recipients must fully comply with all the terms and conditions of their specific allocation of funds or face recoupment of some or all payments. Furthermore, relief fund recipients are subject to review and audit by the HHS inspector general to verify compliance with the various funding terms and conditions.
With deep federal government, health system operational improvement, and policy expertise, Guidehouse was immediately ready and uniquely qualified to help providers in their efforts to secure timely and maximum reimbursement, allowing them to
maintain focus on their staff and communities.
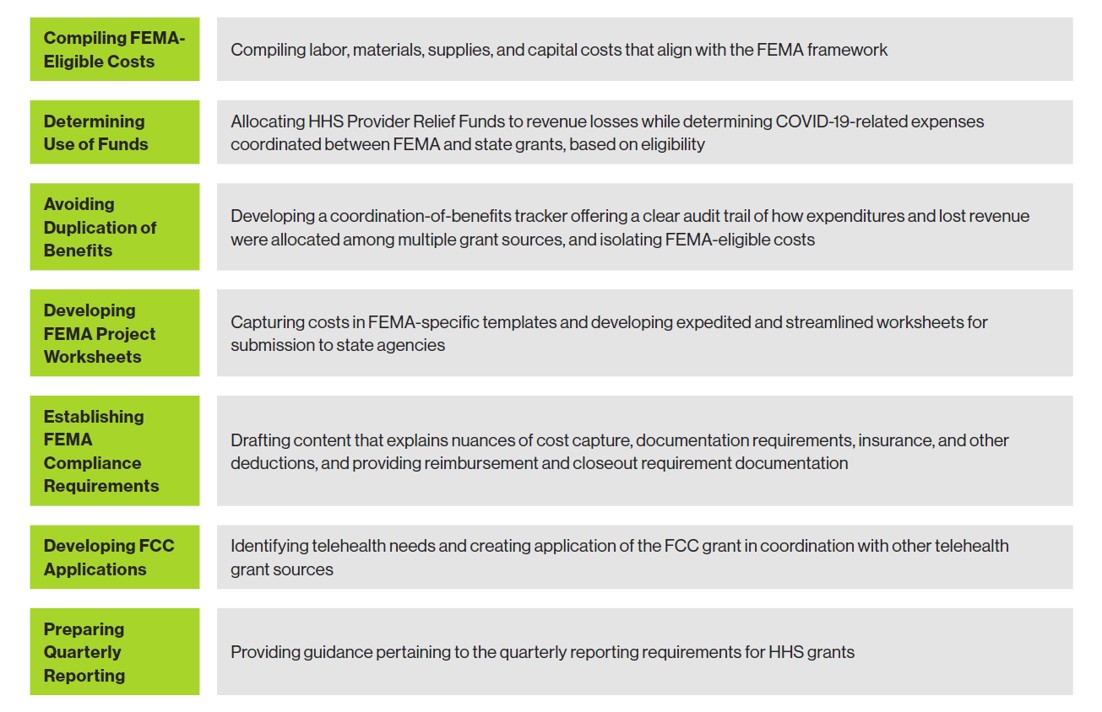
For example, from March 2020 to June 2020, Guidehouse, which has decades of experience managing hundreds of billions of dollars in federal funding disbursement, assisted hundreds of hospitals and health systems with capturing, analyzing, allocating, and submitting well articulated applications for reimbursement via these strategies and tactics:
All clients are also being informed daily of regulatory and policy developments, including federal and state funding opportunities, to assist them in the coordination of benefits and to make informed decisions on their economic recovery. This includes working with health systems to help them identify, understand, and coordinate other COVID-19 recovery programs created by Congress, such as:
To date, Guidehouse has helped hospitals and health systems coordinate more than $2.5 billion in grants and benefits. This includes:
Moving forward, Guidehouse is tracking more than $250 billion in total COVID-19 federal funding for hospitals and health systems across multiple funding mechanisms. This includes helping providers prepare for audits that will require comprehensive supporting documentation for pandemic-related expenditures.
The firm also continues to work with FEMA, the Centers for Medicare & Medicaid Services, HHS, state emergency management leaders, governors, legislators, and more to help shape interpretations and responses and best position clients for success. This includes assisting with policy research aimed at enabling states and providers to develop a more precise and stable response to future disasters that impact the healthcare delivery network.
________________________________________________________________________________________________________________________________________
1. American Hospital Association, “New AHA Report Finds Financial Impact of COVID-19 on Hospitals and Health Systems to Be Over $200 Billion through June,” May 5, 2020, https://www.aha.org/special-bulletin/2020-05-05-new-aha-report-finds-financial-impact-covid-19-hospitals-and-health.
Guidehouse is a global AI-led professional services firm delivering advisory, technology, and managed services to the commercial and government sectors. With an integrated business technology approach, Guidehouse drives efficiency and resilience in the healthcare, financial services, energy, infrastructure, and national security markets.