 Search
Search


As industry consolidation brings more patients to fewer healthcare facilities, a formal capacity management strategy is essential for managing patient placement, improving throughput, and expanding access within hospitals and health systems.
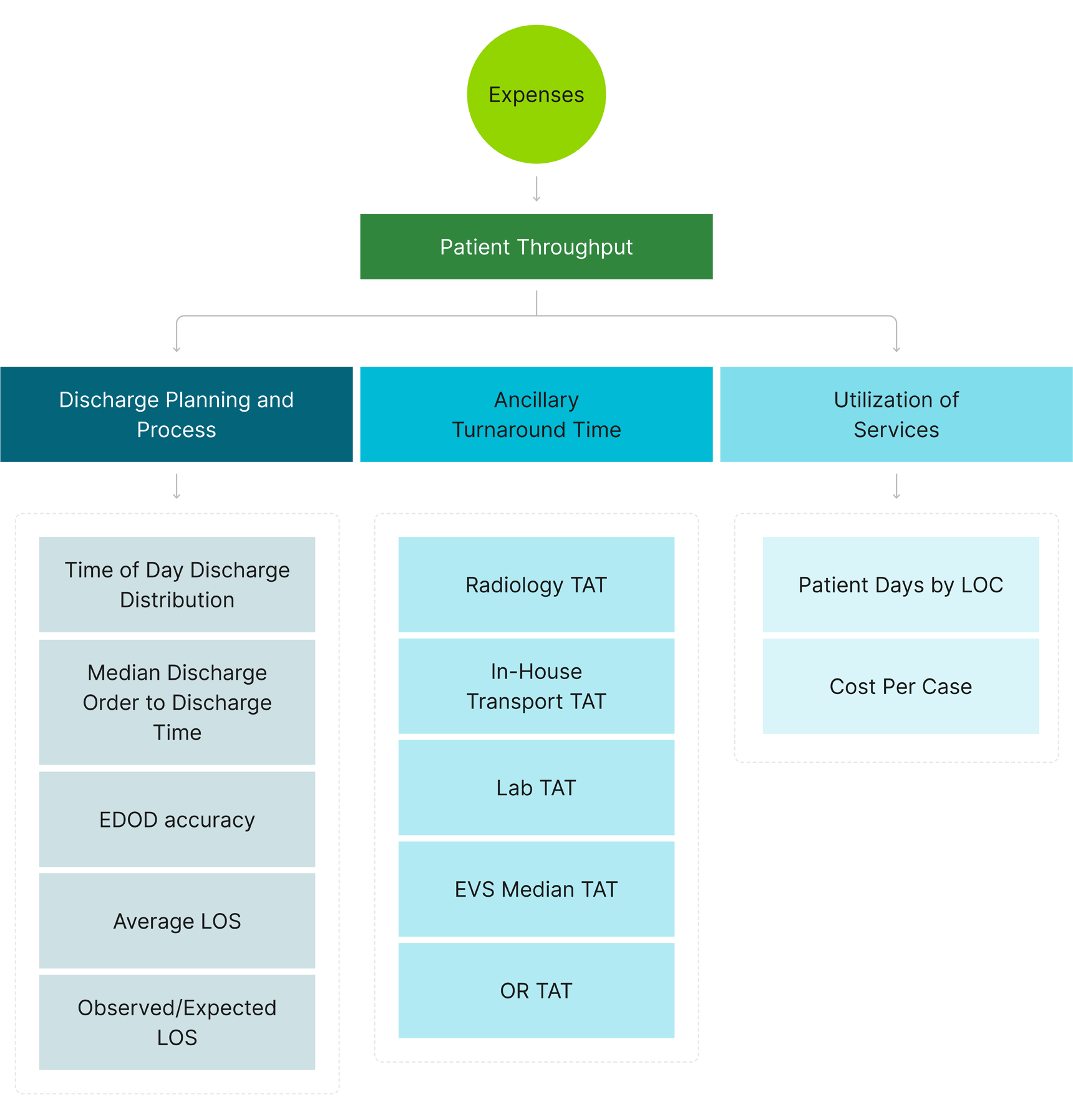
The metrics that help healthcare organizations understand their capacity are complex and come from a wide variety of data sources. The availability of nursing, physician, and ancillary services all play a role in calculating capacity. In any equation, cost and revenue drivers serve as the framework to distill and tie processes to metrics and outcomes.
Hospital and health system capacity command centers function as centralized operations hubs to monitor capacity and manage patient flow. They enable safe, efficient, and appropriate access, logistics, and transport of all patients. Successful deployment is measured at two levels: micro (a single patient’s daily movement) and macro (level-loading patient needs across hospitals, regions, and the enterprise).
When designing a capacity management strategy and considering the benefits of implementing a capacity command center, it’s important to map process drivers to overarching impact measures. Due to the complexities of capacity ecosystems, there can be many primary and secondary impact drivers. Below are sample driver diagrams that offer insight into potential improvements and benefits.
Exhibit A: Example Revenue Driver Diagram
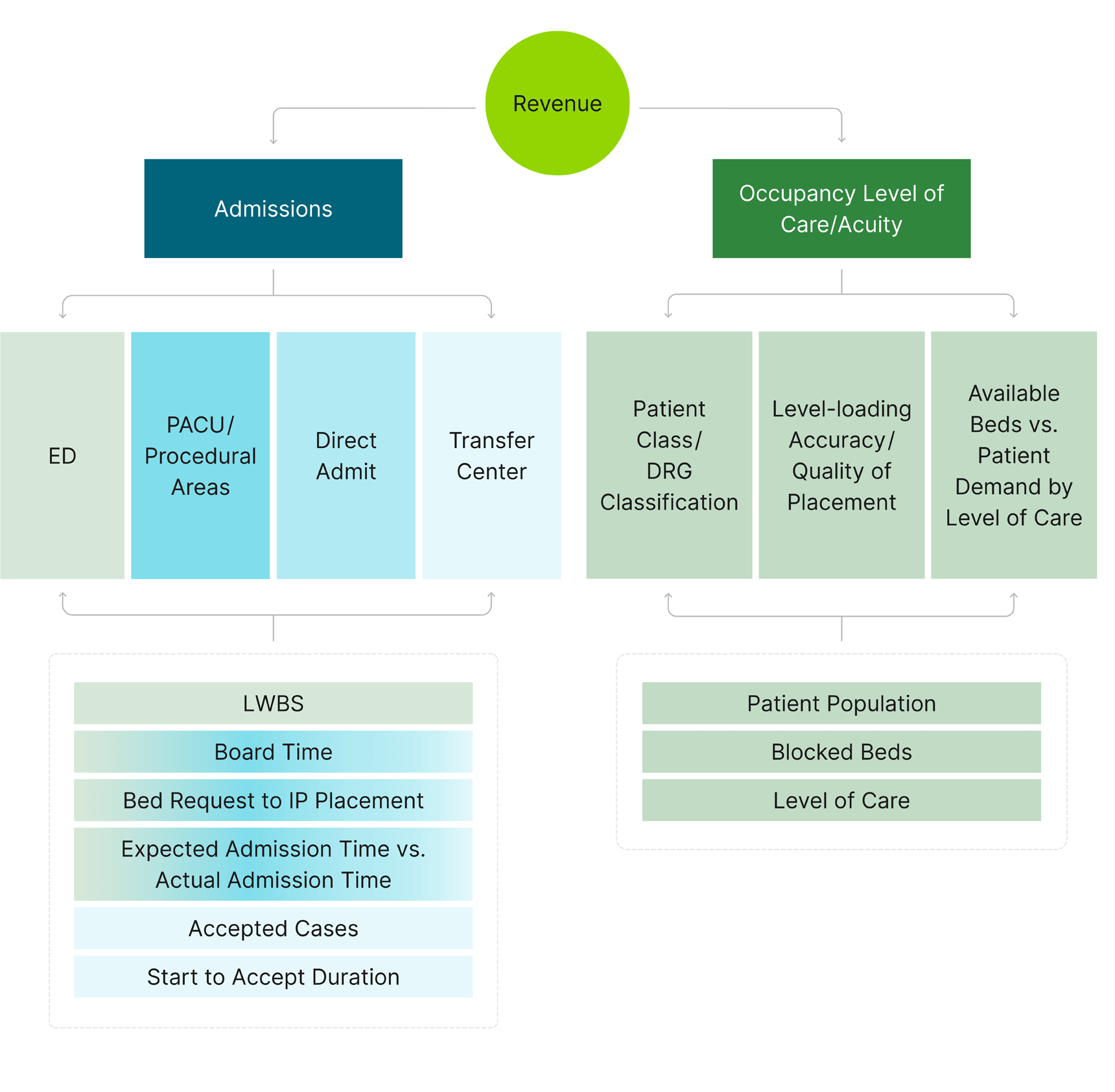
Exhibit B: Example Cost Driver Diagram
A regional, northwest health system engaged Guidehouse on a multiphase capacity management transformation, achieving the following in 12 months:
Guidehouse’s ON TIME approach to capacity management focuses on eliminating silos between departments, strengthening operational processes that impact capacity, and using technology as a tool to maximize both of those efforts. By successfully following this model, healthcare organizations can enhance throughput and improve patient outcomes.
The Fundamentals of ON TIME Care
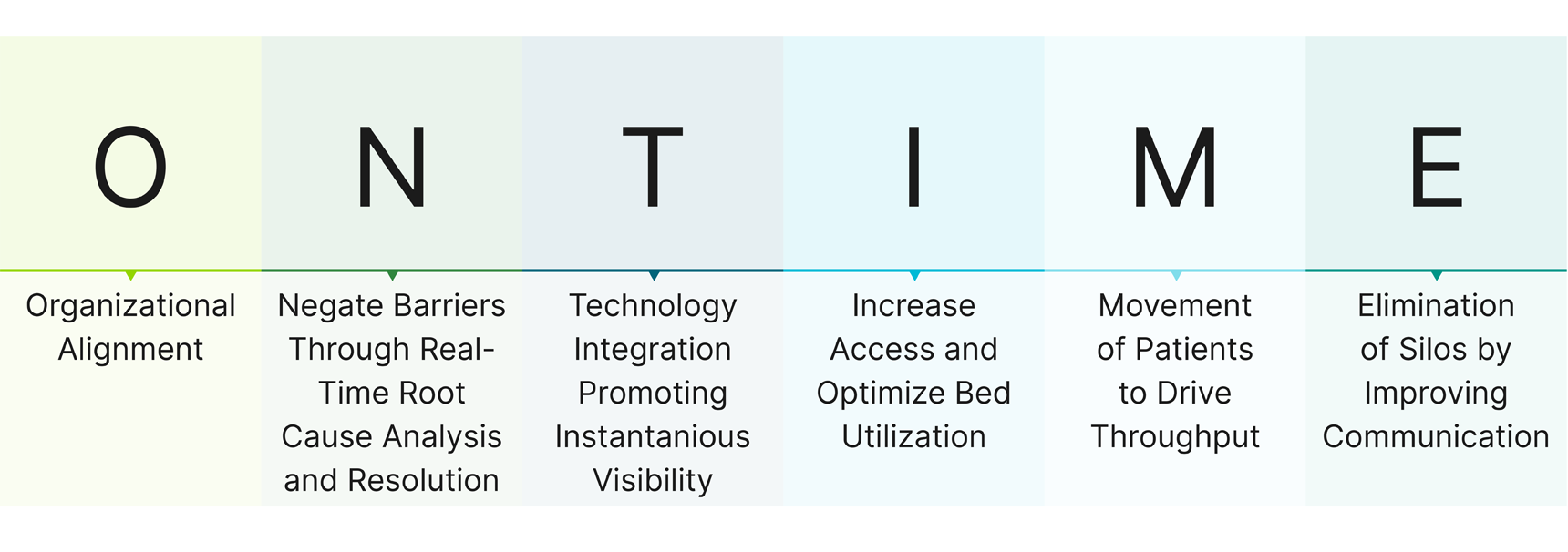
Prior to implementing technology, it's crucial to first address any operational inefficiencies. Simply adding technology to flawed processes can lead to short-term fixes, rather than sustainable improvements that truly enhance care. Our approach focuses on going "back to the basics" to identify and resolve root causes, then operationalizing those solutions while using technology to support seamless, efficient care delivery.
Addressing capacity and throughput with this foundational approach results in a healthy data ecosystem that reaps exponential benefits. This includes:
Dive deep into your current state to understand what processes directly drive value around capacity and patient flow. As you begin to take action, start with these best practices and guiding principles:
Standardize and optimize: Get more patients “in” by first defining how teams will get patients “out” effectively. Start by defining a standard, streamlined approach to patient intake and movement procedures, including intra-hospital movement and all movement after post-acute placement. Create a sense of urgency around early discharges by increasing communication through IT tools, capacity huddle effectiveness, and valuable care team handoffs. Finally, ensure your team is ready to handle challenges, with clearly defined paths of escalation for care delays with alignment of service level agreements.
Build out technology infrastructure: Optimize your EHR facility structure and other technology to reduce technology debt and staff burden. Dashboards that aggregate data from across sources offer staff real-time visibility of KPIs and help leaders identify the root cause of problems. When used with predictive analytics tools, dashboards can help you create net-new models based on historical population health data. Equipped with these insights, leaders can implement a decision support algorithm that assists with triage, prioritization, and clinical placement of patients.
Defer to local experience: A ground-up approach is essential to ensuring cohesiveness between local hospitals and a central command center. Strategies should prioritize local knowledge, leveraging the system command center as a second layer of aid to improve patient flow.
Cultivate experts in capacity management: Leaders should invest in recruiting capacity management experts and training existing staff within multiple levels and disciplines. This should include workflow training and standard operating procedures that focus on reducing the burden on the front lines and staffing wards based on real-time needs.
Develop a governance structure: Your organization should have a capacity management governance structure that supports your strategy, enables scalability and adhere to a repeatable, standardized approach. Regardless of department or service line, capacity-related projects should have common processes, tools, and behaviors. This starts with clearly outlining the roles that leaders within corporate, service lines, hospital, and project management/process improvement have when it comes to capacity management. Performance scorecards can also help ensure a culture of accountability at both the hospital and system levels.
There is no one-size-fits-all approach to building out your capacity management and command center strategy. Guidehouse’s ON TIME care philosophy, coupled with a detailed root analysis, can help healthcare organizations improve access, address the unique concerns of providers, and empower all employees to play a part in achieving operational and financial goals.
Guidehouse is a global AI-led professional services firm delivering advisory, technology, and managed services to the commercial and government sectors. With an integrated business technology approach, Guidehouse drives efficiency and resilience in the healthcare, financial services, energy, infrastructure, and national security markets.