 Search
Search


Access to quality healthcare remains a persistent challenge for rural communities across America. Geographic isolation, workforce shortages, limited financial resources, and aging infrastructure often leave rural hospitals and clinics struggling to sustain essential services. These barriers not only impact patient outcomes but also threaten the economic stability of entire communities that rely on local healthcare systems.
To address these critical issues, the Centers for Medicare & Medicaid Services (CMS) launched the Rural Health Transformation (RHT) Program. This initiative empowers states to redesign rural healthcare delivery by offering flexible payment models, technical assistance, and strategies to strengthen care coordination. By fostering innovation and sustainability, the RHT Program aims to ensure that rural communities have access to high-quality, affordable care while supporting providers in adapting to evolving healthcare demands.
With CMS having recently announced the initial RHT award amounts, state government leaders can start taking action. Understanding how RHT funding works—and where their state stands compared to the application request—is a critical first step.
On December 29, 2025, CMS allocated the first $10 billion of RHT Program funding among each of the 50 state applicants. The map and table below show the state-by-state allocations:
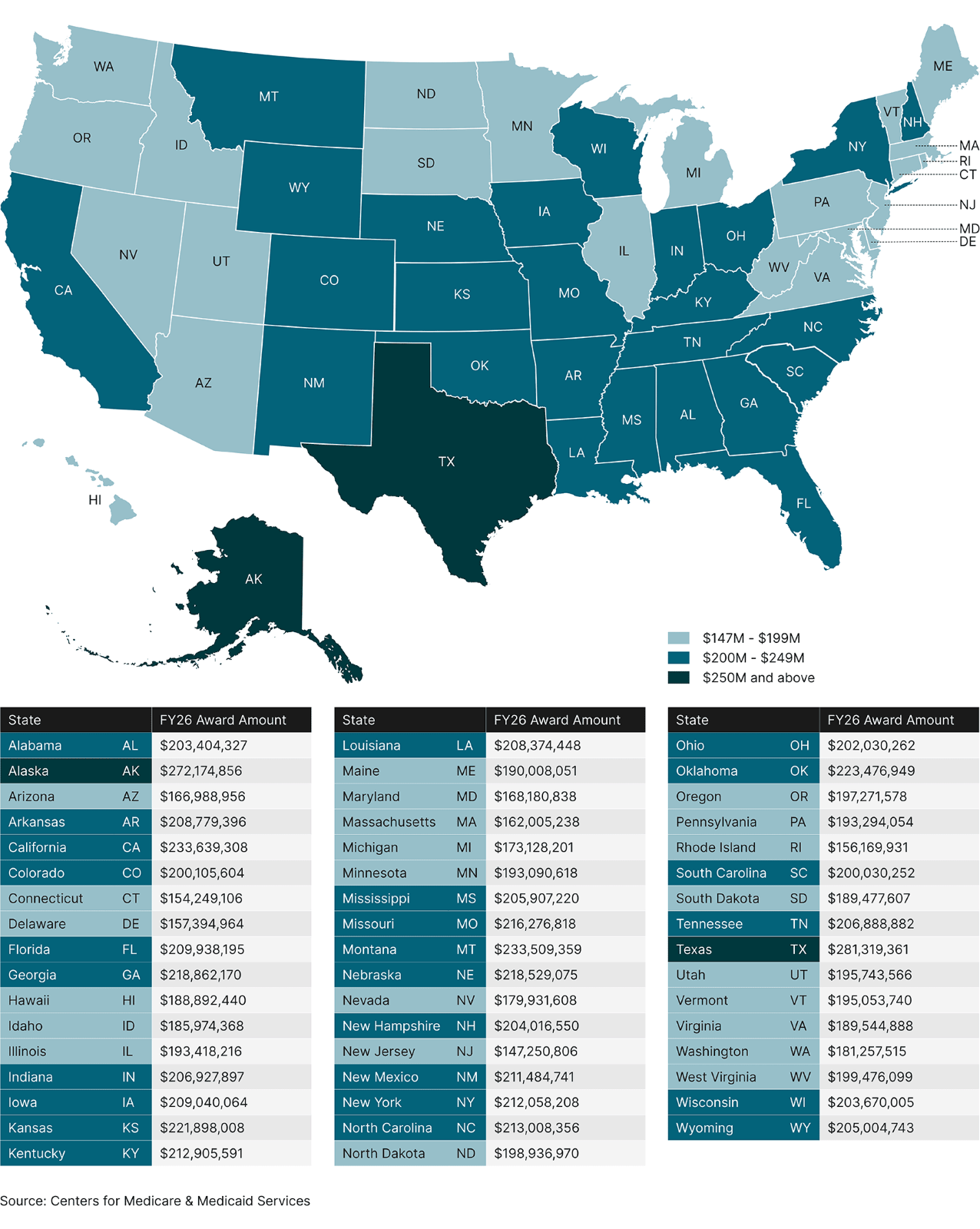
CMS required each state to assume a $1 billion budget over the program’s five-year timeline (i.e., $200 million per year), for planning purposes. Following application submission and review, CMS allocated funding according to the legislative requirements of the RHT Program. The methodology directed CMS to award 50% of funds (i.e., $5 billion in FY 2026) evenly across all applicants and the remaining 50% based on technical scoring factors and each state’s proposed initiatives. As the map above shows, this methodology resulted in some states receiving more than the initially requested $200 million per year (27 states) and some receiving less (23 states).
The healthcare realities and challenges in states such as Texas, Alaska, and California are much different from geographically smaller states. The significant rural and frontier community presence across each of these states presents unique dynamics, with the cost to implement RHT Program initiatives being higher than in other rural communities across the country. For example, the cost to recruit and retain a physician to a remote frontier community in Alaska may be significantly higher than the cost to recruit a similar physician to a rural community in the Southeast. The additional funding that CMS allocated to frontier states may help provide the extra layer of support for successful RHT Program implementation.
Although states with fewer or smaller rural communities, such as New Jersey, Connecticut, or Rhode Island, received less than the initially requested $200 million in FY 2026, those states still received significant funding to address rural healthcare challenges.
Each state will need to adjust the size and scope of its RHT Program application to align with the funding amount granted by CMS. Publicly available RHT Program applications show that states have planned investments across common themes such as technology, workforce development, enhancing access to care, and assistance to stabilize rural healthcare providers.
As states assess the total funding amounts from CMS, they may need to re-evaluate initiative components and priorities to align initial plans with the realities of the allocated funding.
Some states may be able to use additional funding (i.e., funds over initial budget amounts) to enhance the scope of specific planned initiatives. For example, the additional funding may help states expand rural training opportunities to more stakeholders or increase the scope of shared services functions to assist providers to improve financial viability and enhance operational efficiency. States will not be allowed to use additional funding to implement new initiatives that have not been reviewed and approved by CMS.
States that received less funding than initially planned will need to quickly reprioritize and right-size initiatives to align with what is achievable with the allocated funds. State leadership will need to consider how to reconcile what has been communicated with stakeholders with what's actually possible given the reduced funding amount. CMS will expect results that are aligned with the outcome metrics defined in the state’s application and implementation plan through year one reporting, so states will need to make funding re-allocation decisions quickly.
Now that the application process is complete and CMS has allocated funding, states will need to shift focus to achieving outcomes and maintaining compliance with all federal requirements. Application development was a public process that engaged rural communities, rural hospitals, clinics, associations, legislators, payers, potential vendors, and other stakeholders. Interested parties are likely tracking each state’s application and proposed initiatives and will scrutinize how each state ultimately uses funds to support rural communities. Engaged stakeholders will expect states to quickly and efficiently deploy funding shortly after allocation, and they’ll expect those funds to drive positive outcomes.
CMS will also be closely monitoring states’ use of funding. Each state is required to submit an annual report to CMS outlining how the state has used allocated funding and detailing the impact of those funds.
Continued funding is contingent on availability of funds, program authority, satisfactory performance, and compliance with the terms and conditions of the federal award. CMS notes that states must demonstrate “satisfactory progress” to continue receiving funding. The Notice of Award from CMS includes specific reporting terms, conditions, and timelines.
Recent federal grant programs of similar size and scope (e.g., American Rescue Plan Act grant funding) also included a thorough reporting and reconciliation process. States were required to demonstrate how they had used approved funding and to report on the outcomes. States can leverage the lessons learned through recent programs to support successful RHT Program management.
States are now tasked with identifying implementation partners, distributing funds quickly, and ultimately driving outcome improvement aligned with their approved implementation plan and application. States must balance speed to action and funding distribution with thorough grant and budget management that prepares the state to meet all reporting requirements before budget re-evaluation in advance of year-two RHT Program allocations.
Ultimately, the ability of state leaders to navigate the complexities of RHT funding will enable them to set a course for effective implementation that makes a lasting impact on rural Americans’ health.
Guidehouse is a global AI-led professional services firm delivering advisory, technology, and managed services to the commercial and government sectors. With an integrated business technology approach, Guidehouse drives efficiency and resilience in the healthcare, financial services, energy, infrastructure, and national security markets.