 Search
Search


What is “Connected Care"?
Real-time, electronic communication between a patient and a provider, including telehealth, remote patient monitoring, and secure email communication between clinicians and their patients.
In our world filled with public health crises, ever-increasing pressure to reduce healthcare costs, increasing cybersecurity risks, critical workforce shortages, and the transition toward patient-centered models, the need to adopt creative solutions is at the forefront of healthcare leaders’ thinking. As we are seeing during the COVID-19 crisis, patients are increasingly turning to web-based visits and portal-enabled emails for care, and healthcare providers have moved away from paper to adopting electronic health records (EHRs).
Connected care is at the center of this digital health transformation. Described by the Alliance for Connected Care as “real-time, electronic communication between a patient and a provider, including telehealth, remote patient monitoring, and secure email communication between clinicians and their patients,” hospitals and healthcare entities can use connected care to increase their reach into communities and diversify how they deliver care.
While providers have incrementally increased the use of telehealth solutions, a reduction in legislative restrictions combined with new federal funding related to COVID-19 has health systems engaged in a substantial, rapid deployment of digital health. To be successful, providers will need to overcome existing roadblocks to implementing connected care solutions, such as lack of executive sponsorship and commitment, integration, and interoperability with EHRs.
The World of Connected Care
Connected care encompasses everything from a patient portal to remote visits and procedures. Hospitals and healthcare entities can use connected care to increase their reach into communities and diversify how they deliver care. The recent COVID-19 pandemic has shown just how vital connected care is for ensuring continued services. Organizations that were unprepared to quickly move to technology-supported communications and services will be especially hard-hit from a cost and continuity of patient care perspective.
Even under more stable conditions, the need for hospitals and health systems to implement comprehensive connected care services that reduce costs and improve patient outcomes is greater than ever. In fact, approximately 50% of U.S. adults are living with at least one chronic health condition and nearly 59 million Americans live in health shortage areas.2 Connected care improves access to
care, helps providers and patients avoid costly health care services, and increases convenience for patients.
Health systems can increase their reach into communities to both monitor and support patients after post-acute care episodes, and rely on ever-improving, connected technologies to help meet these challenges. According to a study by the American Hospital Association (AHA), 76% of U.S. hospitals connect with the patient and consulting practitioners using video and other technology. An AHA survey revealed that from 2010 to 2017 there was a 41% increase in the use of telehealth solutions.3 With new COVID-19-related federal funding now available and an associated reduction in digital health restrictions, the telehealth number is expected to go up dramatically.

The benefits of connected care services appear to be limitless. Geographically dispersed patient populations benefit from both increased speed and access to care, as well as establishing a continuity of trusted care between patient and provider.
While the benefits of seamless, connected health technologies are numerous, there are challenges. Achieving maturity within healthcare organizations cannot be accomplished in a vacuum and requires collaboration among several key stakeholders. While payers, providers, technology solutions, and their partners work together to ensure a coordinated approach, patients remain at the center of this ever-changing connected care transformation.

Maturing Connected Care Capabilities
An unintended consequence of connected care’s unexpected growth is immediate implementation without the opportunity to thoughtfully plan a strategy for integration, innovation and design, interoperability with other systems, or governance of implemented technologies — all of which will be exacerbated by the COVID-19 pandemic. Failure to implement connected care services through a coordinated, structured, and phased approach ultimately increases waste in resources — human, financial, technological — decreases innovation, market differentiation and integration, and misses opportunities to collect data rich in detail that could support a health system’s ability to transform its resources.
Guidehouse has developed a Connected Care Maturity Model suitable for both government and private sector healthcare organizations (Figure 1). Guidehouse’s framework guides the implementation of connected care services based upon best practices and principles for achieving maturity and maximizing efficiencies in healthcare organizations. The maturity model approach is structured with phased levels, coupled with descriptive elements for each phase of the process to guide users through its application. This solution aids in the standardization of a common language and vision, the development of a structure to prioritize actions, and the determination of successful goals for the organization. Implementing the maturity process can help organizations recognize cost savings, leverage analytics capabilities, increase efficiencies, and more.
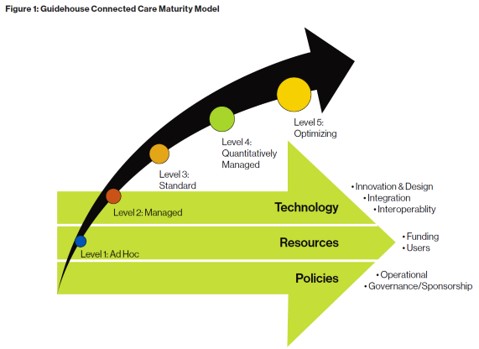
Guidehouse’s model provides healthcare organizations with a road map to move from existing ad hoc approaches toward implementation to ultimately a coordinated, mature organization that maximizes opportunities to meet patients and consumers where they are (Figure 2).

Case Study: Using Connected Care to Reduce Avoidable Hospital Admissions
“Ms. Koro’s ER readmissions for CHF were reduced to zero visits in 2016. Connected care services enabled her to play a more active role in her chronic care management.”
Ms. Koro4 has had chronic congestive heart failure (CHF) for many years. Poorly coordinated and managed care resulted in Ms. Koro making nearly 20 emergency room (ER) visits with acute exacerbations of her disease over a period of 12 months. ER visits for CHF patients increase the length of stay by approximately 0.57 days.5 An enhanced ability to manage her condition and prevent avoidable ER visits would be better for the patient, reduce costs, and reduce the burden on health systems.
Partnering with a connected cardiology group and a skilled home care agency, the health system was able to equip Ms. Koro with remote patient monitoring technology. A tablet with Bluetooth-connected peripherals to detect trending daily changes to her vital signs, weight, and symptoms provided an opportunity to intervene long before Ms. Koro’s symptoms would send her back to the ER.
With this new routine, Ms. Koro’s ER visits and hospital admissions for CHF were reduced to zero visits in 2016. Connected care services enabled Ms. Koro to play a more active role in her chronic care management, as well as incorporate more regular interactions with the health system and its agents to reduce unnecessary visits, resource utilization, and costly readmissions.
As demonstrated in this case study, patient length of stay and ER visits were reduced, which enabled a reduction in costs, allowed for early intervention, improved care coordination and continuum of care, increased patient engagement in her care, and improved overall health.
Stakeholders in the Maturing Model Journey
Throughout a healthcare organization’s maturity journey, leadership should involve a comprehensive change management and culture development program to increase understanding, ownership, engagement, and optimism about the future state of connected care services and the opportunities they provide. As an organization transitions through each phase, it is critical to address technology, resources, policies, and human capital and ensure their participation and support align to achieve the goal of optimizing connected care technologies so that organizations can focus on patient care.
Innovative Collaborators
As connected health technologies become ubiquitous, the need for a thoughtful and phased approach toward implementation and ultimately, optimization, is required. This includes improving care for patient populations and ensuring those who live in remote areas or are unable to have face-to-face visits with their providers are part of the care continuum.
Patients
Throughout the maturity journey, patients must remain at the center to ensure the provision of quality care. Studies show that providing care through connected technologies is promising. During a study in a Las Vegas clinic, an average physician visit was scheduled 18 days from initial request and required two and a half hours of travel to spend approximately 20 minutes with a physician. Using connected care, 79% of patients surveyed report they were able to schedule appointments sooner than 18 days.6

Providers
Providers using connected care solutions are experiencing positive reactions, and two primary factors shown to influence provider adoption of connected care models are empowerment and satisfaction. Provider satisfaction has direct links to both patient satisfaction and patient outcomes. Though connected care encounters produce slightly more paperwork for the provider than a traditional face-to-face visit, studies show that patients resolve 20% more of their issues on average and require fewer follow-up consultations.7 Hospital system-based connected care is found to be the most empowering and satisfying for providers “due to the support system and infrastructure which lead to better appreciation of the utility of telehealth compared to non-hospital-based providers in
an office or clinic setting.”8
Payers
Payer studies show that while the use of connected care may increase utilization slightly, many of the concerns are resolved in a single consultation and new utilization was infrequent. Net savings of a connected care consultation was between $19-$121 per visit over traditional visit costs. Interestingly, 16% of patients9 using connected care report that without it they would not have otherwise sought care, which indicates a new type of utilization.
Emerging Technologies and Ventures
Recognizing that connected care will play a larger role in healthcare, new joint ventures have created innovation within the space. Examples include insurance companies partnering with telecommunications organizations, or internet service providers partnering with healthcare organizations, to develop joint ventures to harness the vast amount of data collected. These joint ventures are creating platforms to empower patients to access their healthcare data and enable them to become active participants in their care journey.
___________________________________________________________________________________________________________________________________________
1. Alliance for Connected Care, “What is Connected Care?,” accessed April 2020, http://connectwithcare.org/what-is-connected-care/.
2. J. Mahar, G. Rosencrance, and P. Rasmussen, “Telemedicine: Past, present, and future,” Cleveland Clinic Journal of Medicine, Volume 85(12), pp. 939-941, December 2018, www.mdedge.com/ccjm/article/189759/practice-management/telemedicine-past-present-and-future.
3. American Hospital Association, “Fact Sheet: Telehealth,” February 4, 2019, www.aha.org/system/files/2019-02/factsheet-telehealth-2-4-19.pdf.
4. Patient’s name has been changed in accordance with Health Insurance Portability and Accountability Act regulations to protect privacy.
5. A. Fischer et al., “The Cost and Length of Stay of Hospital Emergency Department Visits for Chronic Heart Failure Patients in Canada,” Value in Health, pp. A340-341, November 1, 2015,
www.valueinhealthjournal.com/article/S1098-3015(15)02218-4/fulltext.
6. “Managing Satisfaction: What Patients Think of Telemedicine in 2019,” Wheel.com, January 2019, https://www.wheel.
com/blog/telemedicine-patient-satisfaction-studies-2019/.
7. Marie Krousel-Wood et al., “Patient and physician satisfaction in a clinical study of telemedicine in a hypertensivepatient population,” Journal of Telemedicine and Telecare, February 2001, https://www.ncbi.nlm.nih.gov/pubmed/11506755.
8. Sumate Permwonguswa et al., “Provider Satisfaction with Telehealth: Exploring Variation Across Structural and Demographic Factors,” Health Management, Policy & Innovation, March 6, 2018, https://hmpi.org/2018/03/14/provider-empowerment-and-satisfaction-with-telehealth-exploring-variation-across-structural-anddemographic-factors/.
9. Garrison Nord et al., “On-demand synchronous audio video telemedicine visits are cost effective,” The American Journal of Emergency Medicine, Volume 37, Issue 5, May 2019, pp. 890-894, https://www.ajemjournal.com/article/S0735-6757(18)30653-3/fulltext.
Guidehouse is a global AI-led professional services firm delivering advisory, technology, and managed services to the commercial and government sectors. With an integrated business technology approach, Guidehouse drives efficiency and resilience in the healthcare, financial services, energy, infrastructure, and national security markets.