Challenge
Reimbursement and general market changes had Birmingham, Alabama-based UAB Medicine facing multiple revenue cycle management (RCM) challenges at the hospital and physician levels. Although the medical center had a high-performing revenue cycle, leaders knew that continued performance improvement would require a comprehensive focus on RCM enhancement.
They recognized the need for assistance with:
- Improving communication and integration to reduce higher-than-desired initial denials and write-offs
- Accurately measuring and tracking revenue cycle performance
- Enhancing analytical views of reported key performance indicators
- Increasing collaboration between hospital and physician operations within UAB Medicine
Approach
UAB Medicine expanded its partnership with Guidehouse through a comprehensive RCM initiative to improve hospital and physician revenue cycle operations and performance.
The goals of this seven-year effort were to streamline all functions related to medical claim processing and payment and promote greater collaboration, transparency, and consistency.
The initial phase included UAB Hospital and UAB’s faculty practice plan, comprising more than 1,000 physicians across the state.
One of the first steps toward achieving financial improvements was to break down silos—not only between hospital and physician revenue cycle operations but also within each segment. To address this, UAB Medicine established a new RCM governance structure composed of:
- An executive committee responsible for setting and reviewing strategy, operations, and any fundamental changes in governance structure
- A program committee of key stakeholders throughout the system to review ongoing operations, with subcommittees focused on specific areas of opportunity
- A revenue cycle committee responsible for problem awareness, action plans and monitoring, idea sharing and generation, benchmark monitoring, and goal setting
Impact
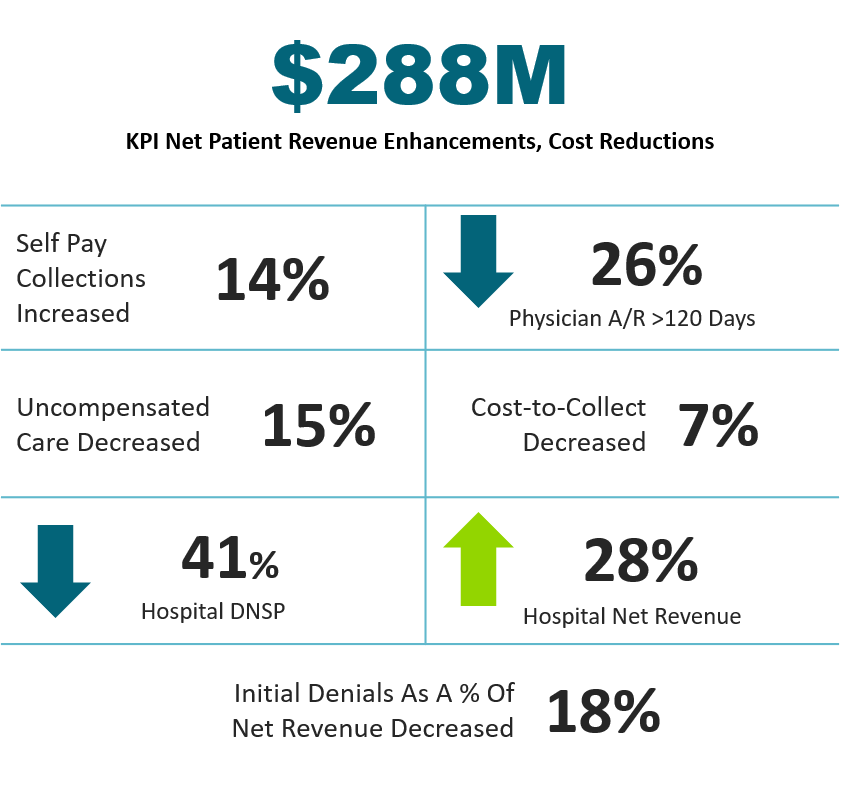
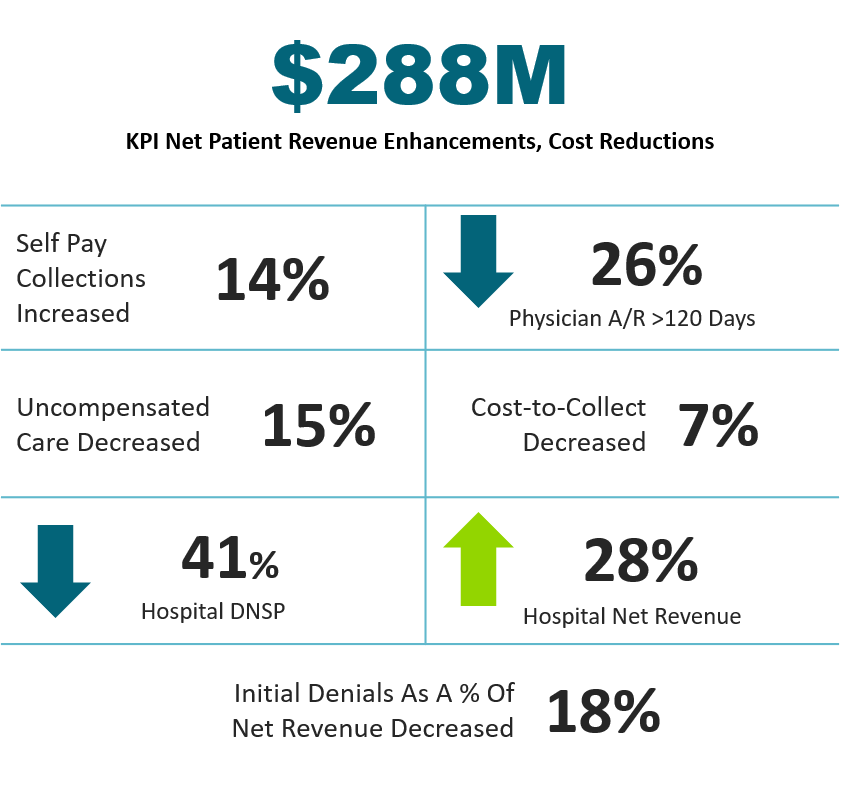
Through this revenue cycle modernization effort, UAB gained the tools and visibility needed to track performance, reduce friction, strengthen accountability, and accelerate cash flow. This resulted in:
- $288 million in net patient revenue enhancements and cost reductions
- Increases in hospital net revenue (28%) and self-pay collections (14%)
- Decreases in uncompensated care (15%), initial denials as a percentage of net revenue (18%), hospital DNSP days (41%), outstanding physician accounts receivable greater than 120 days (26%), and cost to collect (7%)
 Search
Search