 Search
Search


Hospital-at-home models can increase capacity, improve patient experiences, and create market differentiation.
With the Centers for Medicare & Medicaid Services (CMS) Acute Hospital Care at Home Program extension through Dec. 31, 2024, hospitals have an opportunity to better manage capacity while providing better patient experiences. To date, 114 health systems comprising 259 hospitals across 37 states have been approved to participate in the program.
Hospital-at-home programs divert eligible patients into a home setting, thereby improving inpatient capacity, access to care for more patients, and the care experience. These models have been shown to lower the cost of care by approximately 30%.1 Cost savings are achieved by reducing excess inpatient days, decreasing the volume of clinical testing and consultations, and cutting overhead costs.2 Additionally, hospital-at-home models can lower readmission rates and incidences of hospital-acquired infection as well as improve patient satisfaction.
Based on the above operational and quality metrics, Guidehouse analyzed Medicare claims data for hospitals across the country to project the financial impact of implementing the CMS Acute Hospital Care at Home program—including cost savings and revenue opportunities.
Specifically, the analysis identified approximately $4 million in annual opportunities for the average hospital by caring for eligible patients at home, across three areas:

Hospitals that have been approved for the waiver are more likely to have a higher number of Acute Hospital Care at Home-eligible encounters compared to hospitals that have not yet received the waiver.
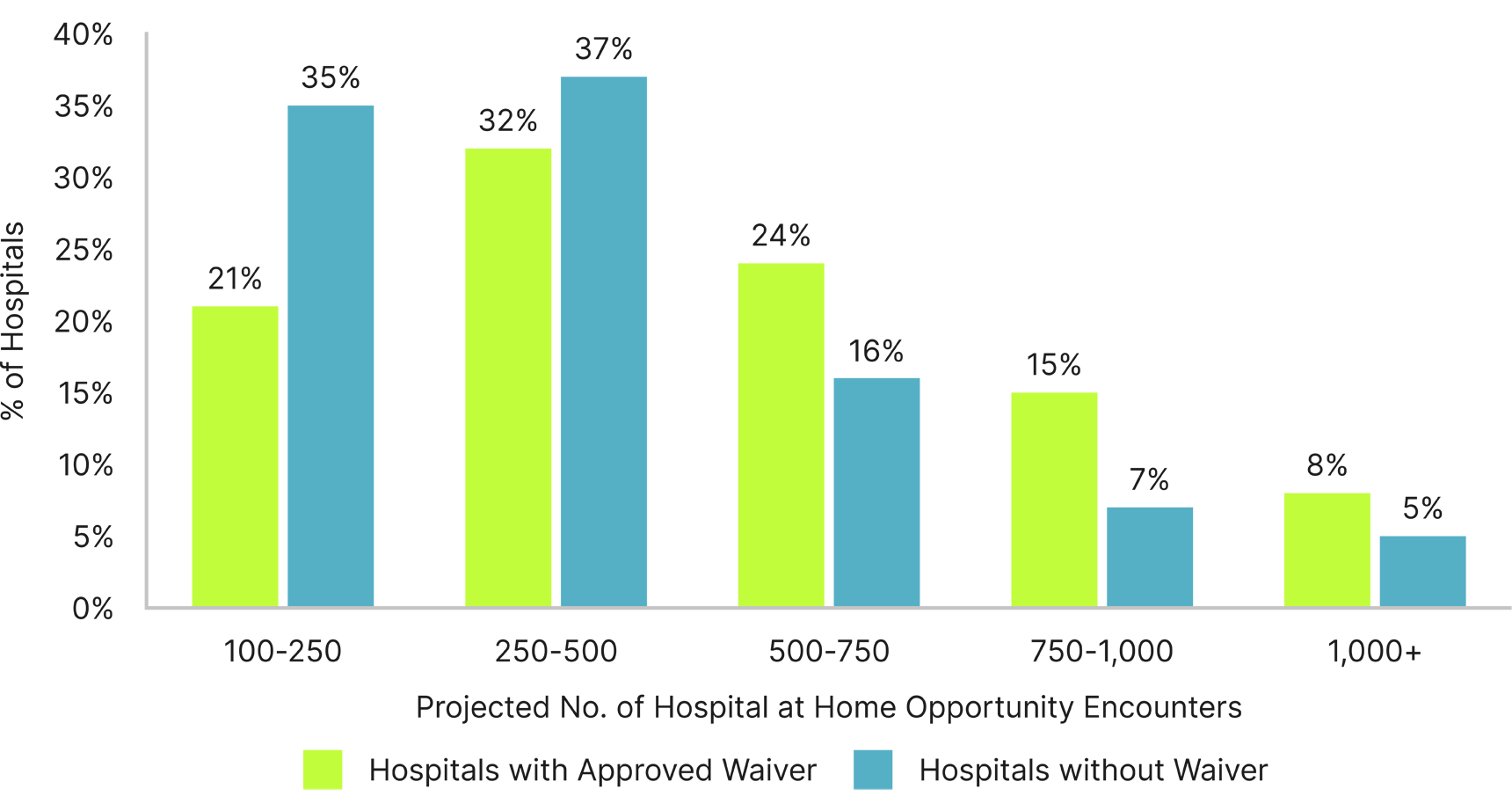
The average length of stay for Medicare admissions is also higher for hospitals that have been approved for the Acute Hospital Care at Home waiver, compared to all other hospitals. Waiver-approved hospitals with more than 750 projected Acute Hospital Care at Home-eligible encounters have an average length of stay that is 8% higher than peer non-waiver hospitals.
The COVID-19 pandemic may have been a driving force behind initial adoption of acute hospital-at-home models, but they provide an innovative approach to solve for many of today’s financial, operational, and clinical challenges. In fact, a survey of more than 130 CEOs found that hospitals are growing their business lines to provide approximately 20% more services outside of the hospital and/or in the home than in 2021.3
However, the level of program implementation varies widely. Some hospitals have their programs up and running, while others have struggled to launch or ramp-up volume.
When leaders at Palomar Health, the most comprehensive healthcare delivery system in northern San Diego County, and a member of the Mayo Clinic Care Network, needed to offer more capacity due to COVID-19 pandemic surges, they engaged Guidehouse to help them achieve CMS Acute Hospital Care at Home waiver approval, as well as build their program in-house via an enterprisewide redesign initiative.4
While Palomar Health was granted CMS Acute Hospital Care at Home waiver approval in just three months, they also worked to redesign their clinical operations strategy to meet the needs of the new model. Key initiatives included aligning acute and ambulatory workflows and integrating them into their EHR. The investment in an innovative and highly technological model has also positioned Palomar Health to mitigate risk and enhance patient safety. Success means that the health system’s goals will have a long-lasting impact on the communities it serves while strengthening its market position.5
With the two-year extension comes an opportunity for hospitals to address capacity issues, improve efficiency, and differentiate their services through improved patient experiences.
It may be time for a hospital-at-home strategy if your organization is experiencing:
Guidehouse is a global AI-led professional services firm delivering advisory, technology, and managed services to the commercial and government sectors. With an integrated business technology approach, Guidehouse drives efficiency and resilience in the healthcare, financial services, energy, infrastructure, and national security markets.